Introduction
An Insurance Claims Management System is a specialized software platform designed to handle the end-to-end lifecycle of an insurance claim. This process begins with the First Notice of Loss (FNOL) and continues through investigation, adjudication, litigation (if necessary), and final settlement. These systems act as a centralized hub, integrating document management, financial tracking, and communication tools to ensure that every stakeholder—from the adjuster to the claimant—is on the same page.
The importance of these tools cannot be overstated. In an era where customers expect Amazon-like speed, manual claims processing is a significant liability. Automated systems reduce the “cycle time” of a claim, identify potential fraud through AI-driven pattern recognition, and ensure strict compliance with varying state and federal regulations. Key evaluation criteria for these tools include the level of automation (touchless claims), integration capabilities with existing policy and billing systems, mobile accessibility for field adjusters, and the robustness of data analytics for loss-reserving accuracy.
Best for: Insurance carriers (P&C, Life, Health), Third-Party Administrators (TPAs), and large MGAs that require a scalable, auditable, and automated way to manage high volumes of claims while maintaining high customer satisfaction scores.
Not ideal for: Small independent insurance agencies that focus solely on sales and distribution without handling the actual adjudication or payout process, or niche providers with extremely low claim volumes who may find the cost of enterprise software prohibitive.
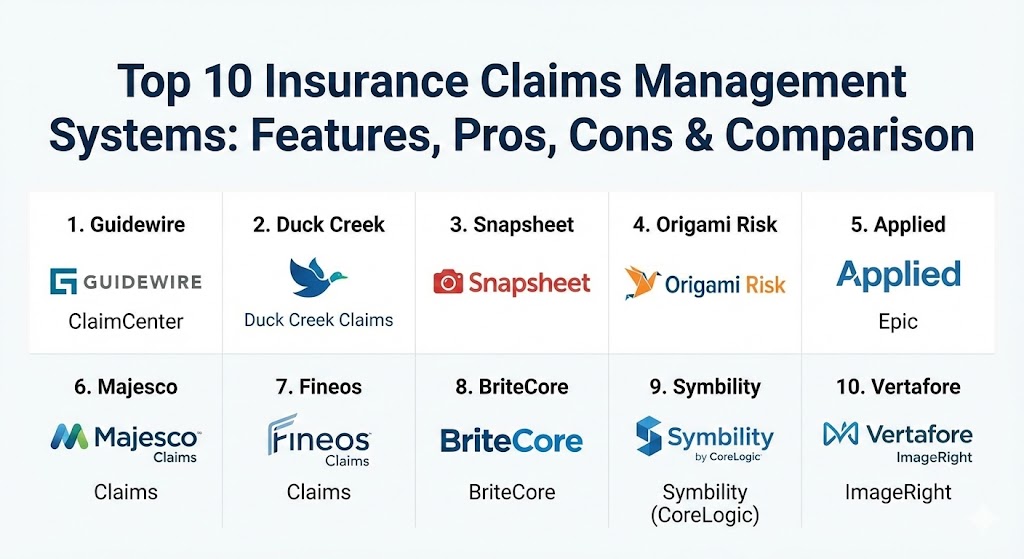
Top 10 Insurance Claims Management Systems Tools
1 — Guidewire ClaimCenter
Guidewire ClaimCenter is widely considered the industry benchmark for Property and Casualty (P&C) claims management. It is a comprehensive system designed to manage the entire claims process for both personal and commercial lines of business.
- Key features:
- Advanced workflow engine that automates task assignment based on adjuster expertise.
- Integrated financial management for accurate loss reserving and payment tracking.
- Robust litigation management tools to track legal expenses and outcomes.
- Seamless integration with the Guidewire “InsuranceSuite” (Policy and Billing).
- Extensive marketplace (Guidewire Marketplace) for third-party data and service integrations.
- Real-time analytics and dashboards for claims performance monitoring.
- Pros:
- Exceptional depth of functionality that can handle the most complex commercial claims.
- Massive global user base and a mature ecosystem of implementation partners.
- Cons:
- High total cost of ownership, often making it a “carrier-only” solution.
- Implementation cycles can be lengthy and require specialized technical resources.
- Security & compliance: SOC 1 & 2, ISO 27001, GDPR, HIPAA, and FIPS-compliant encryption.
- Support & community: World-class enterprise support; Guidewire Education offers extensive certification programs; active “Guidewire Connection” user conferences.
2 — Duck Creek Claims
Duck Creek Claims is a cloud-native, highly configurable claims management solution that emphasizes agility and speed-to-market. It is designed for carriers who want to move away from legacy systems toward a “low-code” environment.
- Key features:
- Low-code configuration tools that allow business users to modify workflows without IT.
- Mobile-first design for field adjusters and claimant self-service.
- Integrated fraud detection and subrogation identification tools.
- Automated document generation and electronic signature integration.
- Cloud-based delivery via Microsoft Azure for high scalability.
- Advanced task orchestration for complex, multi-party claims.
- Pros:
- Extremely agile; updating rules or adding a new line of business is faster than most competitors.
- Modern, intuitive user interface that reduces training time for new adjusters.
- Cons:
- Heavily optimized for the Azure environment, which may limit cloud-agnostic strategies.
- As a “pure” SaaS solution, deep customization can sometimes be more restricted than on-prem alternatives.
- Security & compliance: SOC 2 Type II, ISO 27001, GDPR, and HIPAA compliant.
- Support & community: Robust documentation; Duck Creek University for training; “Duck Creek Idea Exchange” for community-driven feature requests.
3 — Snapsheet
Snapsheet revolutionized the industry by focusing on “virtual appraisal” and digital-first claims handling. It is primarily designed to automate the auto and property claims processes through a mobile-first, cloud-native platform.
- Key features:
- Virtual appraisal tools that allow claimants to submit photos and videos for instant estimates.
- Fully automated “touchless” claims processing for low-complexity losses.
- Integrated payment platform (Snapsheet Transactions) for instant claimant payouts.
- Vendor management portal for direct communication with repair shops.
- AI-driven damage assessment and total loss prediction.
- Omnichannel communication (text, email, app) for real-time claimant updates.
- Pros:
- Drastically reduces cycle times for auto claims, often from days to hours.
- High claimant satisfaction scores due to the streamlined, digital user experience.
- Cons:
- More specialized in auto and property; less comprehensive for complex liability or workers’ comp.
- Smaller enterprise footprint compared to the “Big Two” (Guidewire/Duck Creek).
- Security & compliance: SOC 2 Type II, GDPR, and PCI DSS (for payments) compliance.
- Support & community: High-touch customer success model; agile development cycle with frequent feature releases.
4 — Origami Risk
Origami Risk is a highly flexible, multi-tenant SaaS platform that combines claims management with Risk Management Information Systems (RMIS). It is a favorite among TPAs and self-insured organizations.
- Key features:
- Highly customizable dashboards and reporting for multi-tier organizational views.
- Automated “Action Plans” that trigger tasks based on claim developments.
- Integrated safety and loss control modules to prevent future claims.
- Robust data import/export tools for legacy data consolidation.
- Advanced subrogation and salvage tracking.
- Mobile application for field-based data collection and photo uploads.
- Pros:
- Unrivaled flexibility; the system can be tailored to almost any niche insurance line.
- Consistently ranked highest for customer service and implementation speed in the RMIS/Claims space.
- Cons:
- The interface, while powerful, can feel “data-heavy” compared to more design-focused SaaS apps.
- Complexity can lead to over-configuration if not managed by a skilled admin.
- Security & compliance: SOC 1 & 2 Type II, ISO 27001, HIPAA, and FISMA compliant.
- Support & community: Dedicated service team for every client; extensive online help center and webinar series.
5 — Applied Epic (Claims Module)
Applied Epic is primarily an Agency Management System (AMS), but its integrated claims module is the gold standard for brokers and agencies who need to manage the claims process on behalf of their clients.
- Key features:
- Unified view of policy, billing, and claims data in a single interface.
- Automated “Epic Activities” that track claim progress and follow-ups.
- Integration with carrier portals for real-time claim status updates.
- Document management system specifically built for insurance records.
- Customer portal for claimants to view status and upload documents.
- Integration with CSR24 for 24/7 FNOL intake.
- Pros:
- Eliminates data silos between sales and service teams in an agency.
- Provides brokers with the data needed to advocate for their clients during complex claims.
- Cons:
- Not a standalone carrier system; it is designed to work within the Applied ecosystem.
- Lacks the deep adjudication and payout tools of a dedicated carrier platform.
- Security & compliance: SOC 2, HIPAA, and GDPR compliant via Applied Cloud.
- Support & community: Massive user community (Applied Client Network); extensive training through Applied University.
6 — Majesco Claims Management
Majesco is a leader in digital insurance transformation, offering a claims platform that is part of their broader “Core Suite.” It is designed for P&C carriers looking for a cloud-first, API-driven architecture.
- Key features:
- API-first design that allows for rapid integration with InsurTech ecosystems.
- Embedded AI and machine learning for claim triage and severity prediction.
- Support for “micro-services” architecture to enable specific functional updates.
- Integrated customer “Digital 360” portal for a seamless journey.
- Robust support for diverse lines of business (Personal, Commercial, Specialty).
- Automated compliance tracking for state-specific regulatory forms.
- Pros:
- Excellent for carriers looking to build a modern, “best-of-breed” technology stack.
- Strong focus on the “future of insurance,” incorporating IoT and telematics data.
- Cons:
- Smaller market share in North America compared to Guidewire.
- Requires a strong internal IT or partner team to leverage the API-first capabilities.
- Security & compliance: SOC 2 Type II, ISO 27001, and HIPAA compliant.
- Support & community: Comprehensive “Majesco University”; active participation in industry think-tanks and research.
7 — Fineos Claims
Fineos is the global leader for Life, Accident, and Health (LA&H) claims. Unlike many competitors who focus on property/auto, Fineos is purpose-built for the complexities of disability and life insurance.
- Key features:
- Specialized workflows for Short-Term Disability (STD) and Long-Term Disability (LTD).
- Integrated absence management for employer-paid leave programs.
- Complex benefit calculation engine for variable life and health payouts.
- Robust medical evidence tracking and provider communication tools.
- Automated compliance for FMLA and other regional leave laws.
- High-volume transaction processing for group benefits.
- Pros:
- The undisputed choice for Life and Health carriers; generalist systems often struggle here.
- Deep understanding of the regulatory landscape for employee benefits.
- Cons:
- Not suitable for Property and Casualty (P&C) lines of business.
- The niche focus means a smaller pool of third-party implementation consultants.
- Security & compliance: ISO 27001, SOC 2, HIPAA, and GDPR.
- Support & community: Strong presence in EMEA and North America; localized support teams for regional regulations.
8 — BriteCore
BriteCore is a modern, web-based platform designed for regional carriers and MGAs. It offers a fully integrated suite that includes policy, billing, and claims in a single, user-friendly package.
- Key features:
- Fully browser-based interface requiring no local installation.
- Community-driven development model (shared code for all clients).
- Integrated document management and digital print fulfillment.
- Automated workflow “triggers” for rapid claim movement.
- Native mobile app for adjusters to record voice notes and photos.
- Easy-to-use API for connecting to third-party data providers (e.g., LexisNexis).
- Pros:
- One of the most cost-effective and modern systems for regional carriers.
- The community-funded model means new features are regularly added at no extra cost.
- Cons:
- May lack some of the “deep” enterprise features needed by global Tier 1 carriers.
- Smaller partner ecosystem for specialized custom integrations.
- Security & compliance: SOC 2 Type II, PCI DSS, and HIPAA compliant.
- Support & community: Very active community forum; “BriteCore Community” events for roadmap collaboration.
9 — Symbility (by CoreLogic)
Symbility, a CoreLogic company, is the industry standard for property claims adjusting. It focuses specifically on the estimation and collaboration side of residential and commercial property losses.
- Key features:
- Claims Connect: A cloud-based workflow management hub for all stakeholders.
- Mobile Claims: A powerful offline-capable app for field estimates.
- Integrated aerial imagery and 3D floor plan creation.
- Real-time collaboration between adjusters, contractors, and carriers.
- Deep integration with CoreLogic’s vast property and weather data.
- Automated audit tools for estimate accuracy.
- Pros:
- The best tool for accurate property loss estimating; reduces “leakage” in payouts.
- Essential for managing large-scale catastrophic (CAT) events.
- Cons:
- It is a specialized tool; often needs to be integrated with a broader core system (like Guidewire).
- Can be complex for adjusters who are used to simpler, manual estimating methods.
- Security & compliance: SOC 2, ISO 27001, and GDPR compliant.
- Support & community: Extensive training certifications for adjusters; global support for CAT response.
10 — Vertafore ImageRight
ImageRight is primarily a document management and workflow solution that has become the de facto standard for claims departments at MGAs and agencies that handle heavy paper/digital trails.
- Key features:
- Insurance-specific hierarchical file structure (Policy > Claim > Document).
- Advanced OCR (Optical Character Recognition) for automatic document indexing.
- Visual workflow designer for routing claims through various departments.
- Integration with almost every major Agency Management System.
- Secure “email-to-file” functionality to capture claimant communication.
- Annotations and “sticky notes” for collaborative file review.
- Pros:
- Excellent for managing the massive document trails associated with litigated claims.
- Proven reliability in high-volume, paper-intensive environments.
- Cons:
- It is a workflow/document tool, not a full financial adjudication system.
- The user interface can feel “traditional” compared to modern SaaS platforms.
- Security & compliance: SOC 2 Type II, HIPAA, and GDPR compliant.
- Support & community: Strong user group (NetVU); extensive technical knowledge base and formal training.
Comparison Table
| Tool Name | Best For | Platform(s) Supported | Standout Feature | Rating (Gartner) |
| Guidewire ClaimCenter | Global Tier 1 Carriers | Cloud, On-Prem | Market-Leading Depth | 4.8 / 5 |
| Duck Creek Claims | Agility & Low-Code | SaaS (Azure) | Configuration Speed | 4.6 / 5 |
| Snapsheet | Virtual / Auto Claims | Cloud-Native | Touchless Processing | 4.7 / 5 |
| Origami Risk | TPAs & Self-Insured | SaaS | Extreme Flexibility | 4.8 / 5 |
| Applied Epic | Brokers & Agencies | Cloud, On-Prem | Agency/CRM Integration | 4.5 / 5 |
| Majesco Claims | InsurTech Ecosystems | Cloud-Native | API-First Architecture | 4.4 / 5 |
| Fineos Claims | Life & Health (LA&H) | SaaS | Absence Management | 4.6 / 5 |
| BriteCore | Regional Carriers | Web / SaaS | Community-Led Dev | 4.5 / 5 |
| Symbility | Property Adjusting | Mobile, Web | Accurate Estimates | 4.4 / 5 |
| ImageRight | Document Workflow | On-Prem, Cloud | OCR & Indexing | 4.3 / 5 |
Evaluation & Scoring of Insurance Claims Management Systems
Choosing a claims system is a 10-year decision. We have evaluated these tools using a weighted scoring rubric that reflects the priorities of modern insurance organizations.
| Category | Weight | Evaluation Criteria |
| Core Features | 25% | FNOL, adjudication, payment processing, fraud detection, and reporting. |
| Ease of Use | 15% | User interface, mobile access, training curve, and dashboard clarity. |
| Integrations | 15% | API availability, third-party marketplaces, and legacy system compatibility. |
| Security & Compliance | 10% | SOC 2, HIPAA, encryption, and automated regulatory reporting. |
| Performance | 10% | Uptime, system speed, and scalability during catastrophic events. |
| Support & Community | 10% | Documentation, training, user groups, and vendor stability. |
| Price / Value | 15% | Licensing costs vs. efficiency gains and cycle time reduction. |
Which Insurance Claims Management Systems Tool Is Right for You?
Selecting the right system requires a deep look at your specific business model and volume.
- Solo Agents & Small Agencies: You likely do not need a carrier-grade claims system. Focus on an AMS like Applied Epic, which allows you to track claims and advocate for your clients without needing to manage the actual money movement.
- Small to Medium-Sized Carriers & MGAs: If you are looking for a modern, cost-effective solution that covers the whole lifecycle, BriteCore or Origami Risk offer excellent value with significantly faster implementation times than the industry giants.
- Tier 1 Global Carriers: For high-complexity, multi-national operations, Guidewire ClaimCenter is the safe, proven choice. If your strategy is to be a digital disruptor, Duck Creek or Majesco may offer the architectural agility you need.
- Specialized Providers: If you only handle Life and Health, don’t try to force a P&C system to work—go with Fineos. If your primary business is property adjusting or CAT response, Symbility is non-negotiable for accurate estimating.
- Digital Disruptors: If you want to offer a “touchless” experience where auto claims are paid in minutes, Snapsheet provides the specific AI and virtual tools needed for that specialized journey.
Frequently Asked Questions (FAQs)
1. What is the difference between a Claims Management System and a Policy Administration System?
A Policy Admin system manages the “front end”—quoting, binding, and issuing policies. A Claims system handles the “back end”—the process that occurs after a loss. Many vendors offer both in an integrated suite.
2. Can these systems help detect insurance fraud?
Yes. Modern systems use AI to scan for patterns such as multiple claims for the same loss, suspicious medical provider behavior, or inconsistencies in FNOL data, flagging them for Special Investigative Units (SIU).
3. How long does it take to implement a new claims system?
A regional implementation of a system like BriteCore can take 4–6 months. A full-scale global replacement of a legacy system with Guidewire can take 12–24 months or more.
4. Do these systems support mobile adjusting?
Almost all top-tier systems now offer mobile apps. These allow adjusters to take photos, record voice notes, and even issue payments directly from the field, often without needing a constant internet connection.
5. What are “touchless claims”?
Touchless claims are those processed entirely by software without human intervention. This is common for low-complexity, high-frequency claims like a small auto glass repair or a simple travel insurance delay.
6. Is cloud-based better than on-premise for claims?
Cloud-based systems (SaaS) are generally preferred today because they allow for easier updates, better disaster recovery, and the ability for field adjusters to access data from anywhere.
7. How do these tools help with compliance?
They automate the generation of state-mandated letters (like explanation of benefits), track regulatory deadlines for payouts, and provide the comprehensive audit logs required by state insurance commissioners.
8. Can I integrate third-party data like weather or medical records?
Yes. Modern systems use APIs to pull in weather data (to verify hail or wind claims) or medical records and bills (for health/workers’ comp claims), significantly speeding up the investigation phase.
9. What is “leakage” in claims management?
Leakage refers to money lost through inefficient processing, overpayment of claims, or missed subrogation opportunities. A good system reduces leakage by enforcing strict payment rules and automated auditing.
10. Do these systems handle claimant payments directly?
Many integrated systems now offer “digital disbursements,” allowing carriers to send claim payments instantly to a claimant’s debit card or bank account via services like Snapsheet Transactions or Guidewire’s payment partners.
Conclusion
The insurance landscape is shifting from “indemnification” to “experience.” As claimants demand faster, more transparent service, the role of a robust Insurance Claims Management System becomes central to a carrier’s survival. Whether you choose the massive enterprise power of Guidewire, the digital agility of Duck Creek, or the specialized expertise of Fineos, the goal is the same: to turn a traumatic loss into a managed, efficient recovery. The best tool for your organization will be the one that balances your technical capabilities with your customers’ expectations.